
U.S. maternal mortality points to institutional racism. Is philanthropy listening to Black women?
Maternal mortality is steadily increasing. Is your philanthropy keeping up?
Every year, 700-900 women die of pregnancy related causes in the U.S., one of the worst maternal mortality rates among developed countries.
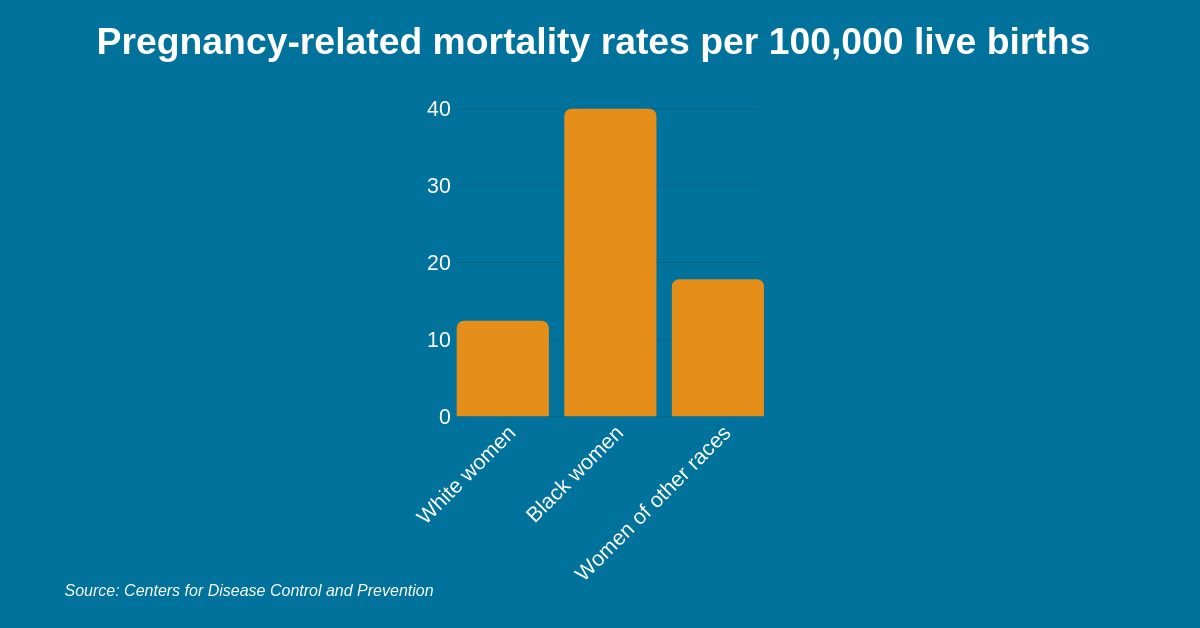
A closer look shows racial disparities carry the statistic: Black women are 3 to 4 times more likely to die of pregnancy related causes than non-Hispanic white women regardless of education and socioeconomic status.
Despite these alarming statistics, philanthropic funding for maternal health has not kept pace with the number of pregnancy related deaths among Black women.
Funders can and should be doing more.
According to the Centers for Disease Control’s latest data, maternal mortality steadily increased between 2011 and 2014 with significant racial disparities: 40 deaths per 100,000 births for Black women compared to 12 per 100,000 births for white women.
In the same period, maternal health funding decreased nearly 32% from $87 million to $58 million.
The rate of maternal mortality and racial disparities point to complex intersections of social determinants and structural inequities that undermine Black maternal health.
However, in 2011 funders designated only $2.5 million specifically to Black maternal health, and that was gutted by more than 50% in 2014.
The maternal mortality crisis is rooted in the marginalization of Black women.
Decreased funding for Black maternal health indicates a gap in grantmaking strategies and the root causes of pregnancy related deaths in the U.S.
Health outcomes are largely tied to social determinants including health and systems services, location, employment, education, race and income.
Maternal health care operates within systems that inherently undervalue Black lives. For most Black women, that means being exposed to multiple forms of discrimination and institutional barriers to quality care, which leads to wide racial disparities.
Black women are more likely to:
- Be uninsured before becoming pregnant.
- Die of conditions related to pregnancy than white women with the same condition.
- Be exposed to environmental risks.
- Receive subpar medical care based on their location.
- Experience racial bias from health care providers.
Curbing maternal mortality requires investment specifically in Black maternal health care and solutions that engage inequities undermining health outcomes for Black mothers and their babies.
Dr. Joia Crear-Perry, founder and president of the National Birth Equity Collaborative, an NCRP nonprofit member said: “What happens when you mention the medical issues and you don’t talk about the social structure, you pick strategies that are not going to allow for ending any kind of inequity.”
Funders can break the mold and save lives.
Black women need systemic change that begins at the community level: access to vital community health centers, paid family leave, patient-centered care and access to health coverage.
Funders can help by:
- Amplifying Black women-led solutions. The maternal health crisis is propelled by anti-Black racism. Philanthropy committed to maternal health equity should engage Black women and their communities as experts by giving them leadership roles in grantmaking strategies that impact their bodies and communities.
- Promoting and investing in community-led organizing, nonprofit advocacy and civic engagement on behalf of Black women. They are the voices of the communities they serve, having intimate and expert knowledge on local resources and how social determinants effect health outcomes. Funding this work builds critical social capital and promotes long-term systemic change that benefits everyone.
- Promoting Black women leadership within health institutions. Diversity in leadership will hold health care providers and institutions accountable to all patients. They can provide the necessary cultural competence to eliminate racial and cultural bias and discrimination in their organizations.
- Defending the Affordable Care Act (ACA). The repeal of the ACA would have devastating implications for millions of people who rely on Medicaid for maternal care and undo the progress it has made towards health equity. Reach out to your nonprofit partners and ask how you can support them in defending the ACA and expanding access to low-income communities.
Maternal mortality in the U.S. reflects a grave injustice to Black women and a deeply flawed health care system. Their voices must be amplified in the fight for health equity.
Nichia McFarlane is NCRP’s events intern. Follow @NCRP on Twitter.